____________________________________________________________________________________________
U
NIVERSITY OF /MINNESOTA
G
RADUATE MEDICAL EDUCATION
EDUCATIONAL
PROGRAM/CURRICULUM
Department of Otolaryngology
Pediatric Otolaryngology Fellowship
This Pediatric Otolaryngology Fellowship Educational Program/Curriculum is intended for use
together with the Graduate Medical Education Institution Policy Manual, available online at
http://z.umn.edu/gmeim. The Institution Policy Manual contains information about benefits,
policies and procedures that apply to all residents and fellows in a training program at the
University of Minnesota. Should information in the Program Manual conflict with the Institution
Manual, the Institution Manual takes precedence.
It is also intended for use with the Department of Otolaryngology Program Policy and Procedure
Manual, available online at: http://www.ent.umn.edu/education/fellowships. The Department
Policy Manual contains information about policies and procedures that apply to all residents and
fellows in a training program in the Department of Otolaryngology at the University of
Minnesota.

i
UNIVE
RSITY OF MINNESOTA OTOLARYNGOLOGY DEPARTMENT
PEDIATRIC OTOLARYNGOLOGY FELLOWSHIP EDUCATIONAL PROGRAM/CURRICULUM
Pediatric Otolaryngology Fellowship Program Mission Statement
______________________________________________________________________
The mission
of the Pediatric Otolaryngology Fellowship is to develop expertise in the diagnosis
and medical/surgical management of complex pediatric patients in the tertiary healthcare
setting.
ii
Table of Contents
Pediatric Otolaryngology Fellowship
Mission Statement i
EDUCATIONAL PROGRAM/
CURRICULUM
Accreditation 1
ACGME Case Log 1
American Board of Otolaryngology 1
Educational Goals and Objectives 2
Patient Care 2
Medical Knowledge 3
Practice Based Learning & Improvement 5
Interpersonal and Communication Skills 5
Professionalism 5
Systems Based Practice 5
Cleft Palate & Craniofacial Clinic 6
Conferences/Courses 7
Research/Scholarly Activity 7
Evaluation 8
Written Evaluations 8
Semiannual Review 8
Components/Principles of Review 8
Possible Outcomes 8
Fellow Evaluation of Faculty and
Rotations 9
APPENDICES
1. Accreditation Status 10
2. ACGME Requirements, Pediatric ENT 12
Direct corrections to:
Program Coordinator
Phone: 612-625-7692
Fax: 612-625-2101
Email: [email protected]
Mailing address:
Otolaryngology
Mayo Mail Code 396
420 Delaware St SE
Minneapolis, MN 55455
1
Pediatric Otolaryngology Fellowship Educational Program/Curriculum
A. EDUCATIONAL PROGRAM/CURRICULUM
ACCREDITATION
The Pediatric Otolaryngology Fellowship Program at University of Minnesota is accredited by
the Accreditation Council for Graduate Medical Education (ACGME. Accreditation status is
included in Appendix 1. Current requirements for accreditation are included in Appendix 2. For
the most up-to-date information visit ACGME's web site, www.acgme.org.
ACGME Case Log
Pediatric ENT fellows must maintain a record of their surgical procedures on the Resident Case
Log System provided by the Accreditation Council for Graduate Medical Education (ACMGE at
www.acgme.org. Contact Faith Courchane, 612-625-7692 or [email protected] if you have
not received initial login and password from ACGME.
Include procedures performed in clinic as well as in the operating room.
ACGME’s Otolaryngology Residency Review Committee highly recommends that
residents/fellows log their cases on a weekly, or more frequent, basis, so that procedures don’t
become lost or forgotten. Residents/fellows are able to view their case logs at any time, and
can correct entries as needed. The Program Director is able to, at any time, review the
operative data submitted by the fellows. A number of statistics regarding operative data are
available on the ACGME web site (password protected for access by residents/fellows and
program directors, including cumulative national medians, means and standard deviations for
each procedure category, subdivided by year of otolaryngology training. Program Directors are
able to scan the case logs of each of their residents/fellows, tagged for procedure experiences 1
standard deviation or more below the national norms per fellow year of training, so they can
tailor rotations accordingly.
Residents/fellows will be able to print out their cumulative operative experiences.
Resident/fellow logging of procedures relies solely on the AMA’s CPT coding system. The
opportunity to use the CPT codes prepares the residents/fellows for coding procedures after the
completion of training.
The one, and significant, deviation from CPT coding rules allows for “unbundling” so that all
procedures or significant segments of such done by each resident/fellow can be captured.
Ample samples of “unbundling” acceptable for resident/fellow reporting purposes have been
placed as a link on the Resident Case Log web site.
Categories of resident/fellow involvement in a surgical procedure include “resident surgeon,”
“assistant surgeon” and “resident supervisor.” Definitions of these categories are available on
the resident case log web site.
AMERICAN BOARD OF OTOLARYNGOLOGY
Board certification, Otolaryngology: Fellows are expected to take the Otolaryngology
certification exam during their fellowship. Fellows will be given time for preparation for and
participation in this examination. Visit the American Board of Otolaryngology web site at
www.aboto.org for the most up-to-date information on requirements and deadlines.
____________________________________________________________________________________________

____________________________________________________________________________________________
2
Pediatric Otolaryngology Fellowship Educational Program/Curriculum
Board certification, Pediatric Otolaryngology: Board certification is not currently available in the
subspecialty of pediatric otolaryngology.
EDUCATIONAL GOALS AND OBJECTIVES
The Pediatric Otolaryngology Fellow will develop their surgical and practice skills to the level
where they will be able to practice independently as a high level specialist in pediatric
otolaryngology. Fellowship goals and objectives are based on achieving competencies in
patient care, medical knowledge, practice based learning and improvement, communication
skills with patients and the rest of the health care team, professionalism and the ability to train
and practice within a complex pediatric health care system. They will demonstrate this primarily
by managing patients in the operating room, clinic and hospital wards. In addition to teaching
residents and medical students and preparing conferences, the Fellow will make certain that the
service runs smoothly, and will delegate responsibility appropriately to junior residents. The
Fellow will meet informally with the Program Director for Pediatric Otolaryngology weekly to
discuss any issues or problems they see developing in the direction of the service. The fellow
will be evaluated quarterly by the pediatric otolaryngology faculty on the written goals and
objectives as listed below. The goals and objectives below apply to both sites (Children’s
Hospitals and Clinics of Minnesota and Masonic Children’s-University of Minnesota Pediatric
patients with the listed disorders are seen and cared for at both sites. The fellow reviews the
surgical schedule at both sites one week ahead of time and than will plan their future schedule
accordingly to obtain and complete their goals and objectives. Outpatient clinic is performed
only at Children’s ENT and Facial Plastic Surgery which is within and attached to Children’s
Hospital of Minnesota. Children’s Hospitals and Clinics of Minnesota and the University of
Minnesota Masonic Children’s Hospital are approximately three miles apart.
Patient Care: The Fellow must:
Demonstrate ability to manage the Pediatric Otolaryngology Service, including:
Direct residents and coordinate nursing, social services and administration to optimize
patient care.
Care for patients in the pediatric, cleft, craniofacial, tumor board, Velocardiofacial, and
vascular anomalies clinics.
Develop the treatment plan for all patients undergoing medical or surgical care on the
Service.
Direct the presentation of appropriate patients to the Pediatric Head and Neck Tumor
Board.
Demonstrate practice based learning by evaluating and effectively critiquing the current
medical literature related to patient care
Demonstrate effective communication with the health care team and the patient and the
patient’s care givers.
Demonstrate professional behavior at all times through communication and knowledge
with the patient and their family.
Demonstrate and be aware of cost effective management for a particular patient’s care
as well as possible ethical or medical-legal issues.

Pediatric Otolaryngology Fellowship Educational Program/Curriculum
____________________________________________________________________________________________
3
Medical Knowledge: The Fellow must:
Demonstrate superior medical knowledge, equal to the faculty, regarding all aspects o
f
pediatric otolaryngology (otology, head & neck, bronchoesophagology, craniofacial &
cleft palate /
lip, facial plastics, laryngology and rhinology), including the following:
Ear
Pathophysiology in children of: otitis media, otitis externa, otorrhea, hearing loss, vert
igo,
tinnitus, Eustachian tube dysfunction, mastoiditis, intracranial suppurative complications,
temporal bone tumors
Nose, paranasal sinuses, face and or
bit
Pathophysiology in children of: nasal obstruction, rhinorrhea,
epistaxis, associated
orbital infe
ction, cosmetic nasal deformity, allergies, sinusitis,
tumors of the paranasal
sinuses
Mouth, Pharynx and Eso
phagus
Pathophysiology in children of: pharyngitis, tonsillitis, dysphagia, congenital
malformatio
ns, cleft lip and palate, inflammatory
disorders, salivary gland disorders,
tumors of the mouth and pharynx, trauma to pharynx and esophagus, foreign bodies of
the mouth and pharynx.
Larynx, Trac
hea, Bronchi and Lungs
Pathophysiology in children of: cough, aspiration, hoarseness, stridor, airw
ay
obstruction, congenital malformations of the airway, infections of the airway, neurologic
disorders of
the airway, tumors of the respiratory tract, trauma to the
airway, foreign
bodies, airway reconstruction
Neck
Pathophysiology in children of: neck masses, developmental anomalies,
adenopathy,
injuries and
trauma, tumors (benign
and malignant)
Communication Disorder
s
Pathophysiology in children of: language and speech disorders, cleft lip and palate,
velopharyng
eal insufficie
ncy.
The Fellow must demon
strate ability to perform:
Laryngobronchoesophagology in premature neonates, neonates, infants and childr
en.
Head and neck surgery including salivary, endocrine, lymphovascular an
d neck
dissections in children as well as demonstrate capabilities in the latest endoscopic
techniques
in head and neck surger
y,
Care for patients with co-morbidities, including cardiac, hematology-oncology and both
solid organ and bone marrow transplants ,
Laryngotracheal surgery both open and endoscopic techniqu
es,
Otologic surgery including cochlear implants, and reconstruction for cong
enital
malformatio
ns
Surgery of the nose and
paranasal sinuses,
Surgery for congenital abnormalities of the head
and neck,
Surgery for benign and malignant head and neck disorders.
Pediatric Otolaryngology Fellowship Educational Program/Curriculum
____________________________________________________________________________________________
4
Pediatric facial plastics including cleft lip and palate, mandibular advancement and
rhinoplasty
Although the majority of the Fellow’s time is spent at Children’s Hospital and Clinics of
Minnesota, the addition of University of Minnesota Masonic Children’s Hospital provides access
to an expanded patient base, especially in the area of otology, thus broadening the educational
opportunities available to the fellow. Masonic Children’s Hospital includes the Lions Children’s
Ear Clinic where approximately 50 pediatric cochlear implants are done per year by the pediatric
otolaryngology service in addition to numerous complex pediatric otologic cases located at this
site. Additional patients include children with airway reconstructive needs, cystic fibrosis, bone
marrow transplantation and patients with complex pediatric head and neck tumors. The fellow
averages about 2 cases per week at this site.
At Masonic Children’s Hospital, the fellow will have additional opportunities to demonstrate
superior medical knowledge in the areas of:
Pathophysiology in children of: otitis media, otitis externa, otorrhea, hearing loss, vertigo,
tinnitus, Eustachian tube dysfunction, mastoiditis, intracranial suppurative complications,
temporal bone tumors
And to demonstrate the ability to perform:
Otologic surgery including cochlear implants, and reconstruction for congenital
malformations
Benchmarks for the Maturation of the Pediatric Otolaryngology Fellow
At both sites, the Fellow should show increasing skill and knowledge in the care of patients, in
the doctor-patient relationship, in the use of diagnostic and therapeutic aids and methods, in the
ability to form accurate diagnoses and institute appropriate treatment, in the use of medical
literature, in the desire and ability to research problems areas and in teaching.
Specific and in-depth knowledge of the following subjects, as related to the entire body, with
emphasis on the head and neck, bronchopulmonary, otologic and esophageal areas should
increase during the training period:
Allergy
Anatomy
Anesthesia-both local and general
Audiology
Biochemistry
Clinical pathology
Embryology and developmental defects
Histology
Histopathology
Microbiology and microbiopathology
Physiology
Oncology
Radiographic anatomy and diagnosis
Surgical development ultimately should satisfy these critical performance requirements:
1. Eliciting historical information
2. Obtaining information by physical examination
3. Obtaining and interpreting x-rays
Pediatric Otolaryngology Fellowship Educational Program/Curriculum
____________________________________________________________________________________________
5
4. Obtaining additional information by other means
5. Approaching diagnosis objectively
6. Recognizing condition
7. Adapting treatment to the individual case
8. Determining extent and immediacy of therapy needs
9. Obtaining consultation on proposed treatment
10. Planning the operation
11. Making necessary preparations for operating
12. Performing the operation
13. Modifying operative plans according to situation
14. Handling operative complications
15. Instituting a non-operative therapy program
16. Handling patient
17. Performing emergency treatment
18. Paying attention post-operatively
19. Monitoring patient's progress
20. Providing long-term care
21. Showing concern and consideration
Practice Based Learning and Improvement: The Fellow should demonstrate the ability to:
Evaluate and effectively critique published literature in critically acclaimed journals a
nd
texts.
Apply clinical trials data t
o patient management.
Lead acade
mic and clinical discussions.
Attend and actively participate and direct teachin
g conferences.
Interpersonal and Communication Skills: The Fellow should:
Establish and maintain professional and therapeutic relationships with p
atients and
healthcare team members.
Manage and maintain efficiency of the team (O.R. team, ward team, clinic team).
Teach residents, medical students, nurses, and physician assistant students.
Professionalism: The Fellow should:
Demonstrate behaviors that reflect an ongoing commitment to continuous profession
al
development, ethical practice, sensitivity to diversity and responsible attitudes.
Actively seek and be receptive to feedback on pe
rformance.
Be attentive to ethical
issues.
Be involved in end-of-life discussions and decisio
ns.
Be sensitive to gender, age, race, and cultural
issues.
Demonstrate leadership.
Systems Based Practice: The Fellow should:
Be aware of cost-effective care issu
es.
Be sensitive to medical-legal issues.
Use information technology/comput
er resources.

____________________________________________________________________________________________
6
Pediatric Otolaryngology Fellowship Educational Program/Curriculum
Sample of Goals and Objectives For One Assignment
CLEFT PALATE AND CRANIOFACIAL CLINIC
Patient Care
Direct residents and coordinate nursing, social services an
d administration to optimize
patient care.
Care for patients in the pediatric, cleft, craniofacial clin
ics.
Develop the treatment plan for all patients undergoing medical or surgical
care on the
Service.
Direct the presentation of appropriate patients to the multidisciplinary board during t
he
clinic.
Demonstrate practice based learning by evaluating and effectively critiquing the curr
ent
medical literature related to patient care
Demonstrate effective communication with the health care team and the patient and
the
patient’s
car
e givers.
Demonstrate professional behavior at all times through communication and knowle
dge
with the patient and their
family.
Demonstrate and be aware of cost effective management for a particular patient’s car
e
as well as p
ossible ethical or medical-legal issues
.
Medical Knowledge
Demonstrate superior medical knowledge, equal to the faculty, regarding all aspects o
f
pediatric cra
niofacial & cleft palate / lip, and facial plastics.
Demonstrate the ability to present above knowledge to the multidisciplinar
y board.
Translate such knowledge in layman terms to the patient’s family.
Demonstrate staff level of knowledge of involved genetics and associated syndromes.
Demonstrate staff level of knowledge regarding associated embryogene
sis of
craniofacial disorders.
Practice Based Learning and Improvement
Evaluate and effectively critique published literature in critically acclaimed journals a
nd
texts regarding cleft lip /
palate and craniofacial disorders and
apply that knowledge
during the weekly multidisciplinary conference.
Apply clinical trials data t
o patient management.
Lead academic and clinical discussions during the weekly multidisciplinary conference.
Attend and actively participate in the multidiscipl
inary conference.
Interperson
al and Communication Skills
Establish and maintain professional and therapeutic relationships with p
atients and
healthcare t
eam members of the clef
t / craniofacial team.
Manage and maintain efficiency of th
e team.
Teach residents, medical students, nurses, and physician assistant students.
Translate difficult terminology into layman’s terms for the patient and care
giver.
Pediatric Otolaryngology Fellowship Educational Program/Curriculum
____________________________________________________________________________________________
7
Professionalism
Demonstrate behaviors that reflect an ongoing commitment to continuous profession
al
development, ethical practice, sensitivity to diversity and responsible attitudes.
Actively seek and be receptive to feedback on performance from the cleft / craniofacia
l
team.
Be attentive to ethical
issues.
Be involved in decision making to avoid potentially serious
or poor outcomes.
Be sensitive to gender, age, race, and cultural issues.
Demonstrate leadership within the clinic and team.
Systems Based Practice
Be aware of cost-effective care issues regarding cleft / craniofacial care.
Be sensitive to medical-legal issues
.
Use information technology/computer resources extensively
and effectively.
CONF
ERENCES/COURSES
Orientation: New fellows are required to attend University of Minnesota Medical School
Resident/Fellow Orientation.
Pediatric ENT Conference /Resident Case Presentation, Fridays, 6:30 a.m., Childrens
The pediatric ENT fello
w presents one to three interesting cases at the weekly pediatric
otolaryngology resident conference. Each week, the core otolaryngology resident on the
pediatric ENT rotation formally presents a case and related literature to the fellow and staff. The
fellow provides feedback to the ENT resident.
Pediatric ENT Pre-op Conference, Wednesdays, 6:30 a.m., Childrens
ENT Resident Core Conference - weekly, Tuesd
ay, 6:30 a.m., University
The pediatric ENT fellow participates when these conferences are devoted to pediatric
topics.
Morbidity and Mortality Conference, monthly, first Tuesday, 6:30 a.m., University
Web-based
Learning, provided by the American Society for Pediatric Otolaryngology (ASPO)
monthly.
Visiting Professors, 6:00 p.m., University, four to six times per year
Resident/Fe
llow Graduation Scientific Program, annually, June
RESE
ARCH/SCHOLARLY ACTIVITY
A research project is required during the fellowship program, and must be approved by Program
Director, Brianne Roby, M.D.

____________________________________________________________________________________________
8
Pediatric Otolaryngology Fellowship Educational Program/Curriculum
EVALUATION
See Also Institution Policy Manual, http://z.umn.edu/gmeim, Evaluation Policy.
Written Evaluations
Evaluations of the fellow are done quarterly by the pediatric otolaryngology faculty through the
online system, where they are available to the director of the pediatric otolaryngology fellowship
for review. The director then meets with the fellow quarterly on an informal basis to discuss the
fellow’s progress and review the case logs.
Semi-Annual Performance Review
The fellowship director meets with the fellow semiannually for a formal review and documents
this meeting in writing. The fellowship director’s summary of the semi-annual review is signed
by both the director and the fellow. The written notes are kept the fellow’s file.
Components/Principles of the Review
All relevant aspects of fellow progress are considered by the faculty/program director at the time
of the review. Review will consider progress toward the goals listed on pages 2 through 7, and
will include:
Clinical and surgical performance and progress: Faculty submit written evaluations
quarterly using the online system.
Research/publication progress
Administrative skill and experience
Teaching skill and experience: Residents submit written evaluations of fellow teaching
using the online system.
Attitude
Punctuality
Conference attendance, participation and presentation
The faculty assume a fellow's performance will mature as the fellow gains greater education and
experience. Therefore, expectations for the fourth-quarter fellow are different from those for the
first-quarter fellow.
Possible Outcomes
Positive outcomes of the Fellow Review include:
Affirmation of good clinical progress
Recommendation for graduation from the program
Information becomes part of the fellows’ permanent file
Negative outcomes of the Fellow Review include:
A reprimand related to concern about performance
Meetings at six-week intervals to evaluate improved performance until the next
scheduled evaluation
Probation for a period of months to allow performance to improve
Expulsion, conducted according to the University of MN appeals process
Information becomes part of the fellows’ permanent file

____________________________________________________________________________________________
9
Pediatric Otolaryngology Fellowship Educational Program/Curriculum
Fellow Evaluation of Faculty and Rotations/Training Program
At the end of each clinical rotation, fellows have the opportunity to evaluate the rotation and the
faculty using the confidential, online evaluation system. Residents/fellows will receive email
reminders when evaluations are due. This information is valuable to improving our program and
residents/fellows are encouraged to complete it.
Fellows can also review evaluations of their own progress submitted by faculty and ancillary
personnel through the evaluation system.
New Innovations Residency Management Suite (RMS is located at www.new-innov.com.
If you don't know your user name or password, contact Faith Courchane, 612-625-7692 or
[email protected]. Institution is “mmcgme.” You may use the "NET" (not enough time
feature to delete evaluations that have been inappropriately assigned to you.
2882631016 - UNIVERSITY OF MINNESOTA PROGRAM
Pediatric Otolaryngology - Minneapolis, MN
Back To Search
Children's ENT and Facial Plastic Surgery
Children's Specialty Center, Suite 450
2530 Chicago Ave S
Minneapolis, MN 55404
http://www.ent.umn.edu/education/pediatric-otolaryngology/index.htm
Specialty:
Pediatric otolaryngology
Sponsoring Institution:
[ 269501 ] University of Minnesota Medical School
Core Programs:
[ 2802631055 ] University of Minnesota Program (Otolaryngology)
Phone:
(612) 874-1292
Fax:
(612) 874-0985
Email:
Brianne B Roby, MD
Program Director
Director First Appointed:
July 27, 2016
Sacha Brueggemann
Phone:
(612) 625-7692
Email:
Original Accreditation Date:
July 01, 2012
Accreditation Status:
Continued Accreditation
Effective Date:
January 26, 2018
Accredited Length of T raining:
Accreditation Council for Graduate Medical Education (ACGME) - Public
Legend
Clinical Site
Primary Clinical Site
Director Information
Coordinator Information
Accreditation And General Information
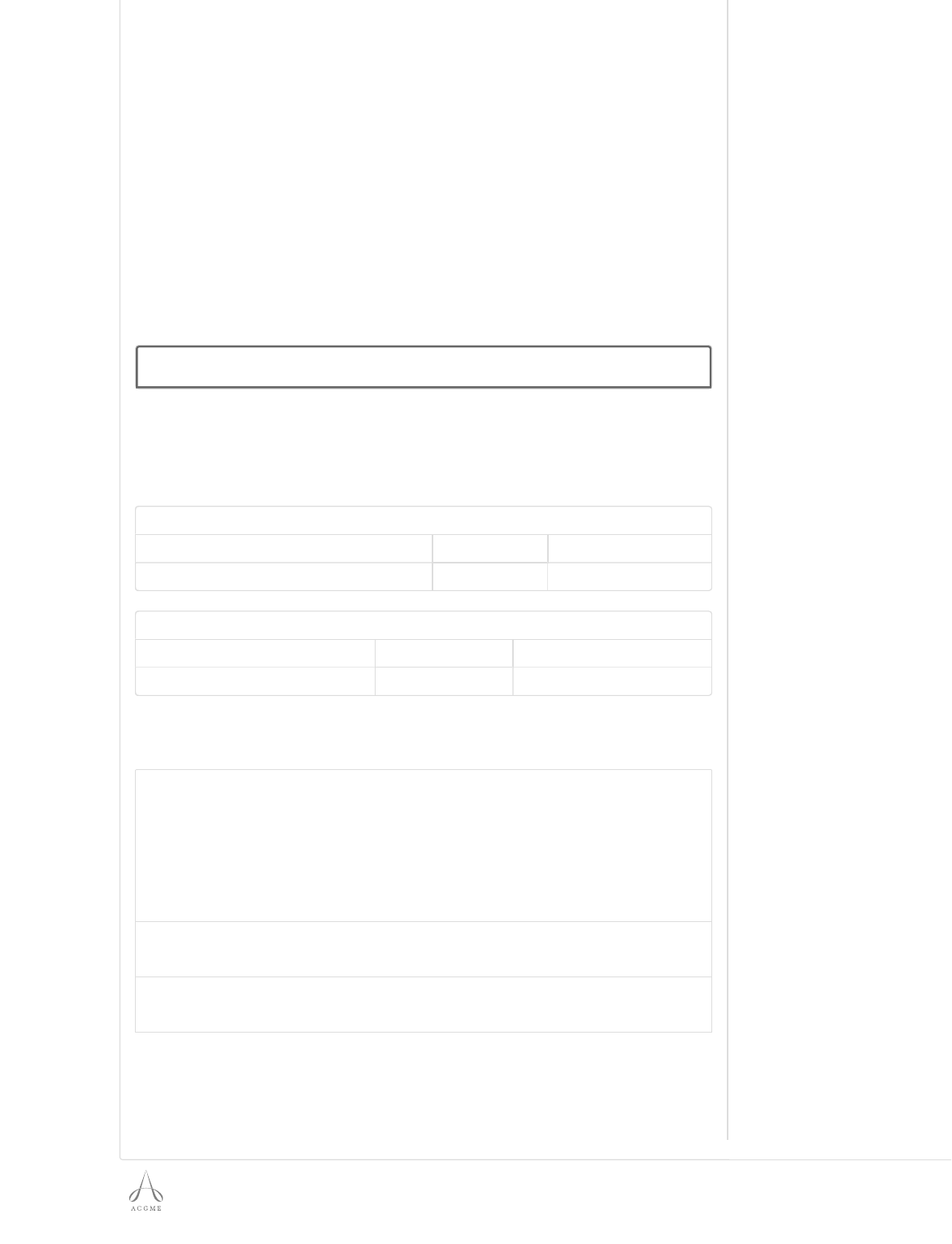
© 2018 Accreditation Council for Graduate Medical Education (ACGME)
1 years
Osteopathic Recognition:
No Information Currently Present
Osteopathic Recognition Effective Date:
No Information Currently Present
Director of Osteopathic-Focused Education:
No Information Currently Present
Last Site V isit Date:
April 16, 2014
Date of Next Site V isit (Approximate):
No Information Currently Present
Self Study Due Date (Approximate):
August 01, 2020
10 Year Site V isit (Approximate):
February 01, 2022
Total Approved Resident Positions:
1
Total Filled Resident Positions*:
1
Complement Breakdown: Approved
Years: 1 Total
Approved: 1.0 1.0
Complement Breakdown: Filled
Years: 1 Total
Filled: 1.0 1.0
*Total filled will reflect the previous academic year until the annual update is completed for the
current academic year. Totals may vary from year to year due to off cycle residents.
Participating Site Information
Showing 1 to 2 of 2 entries
# ID Site Name
Required
Rotation
Rotation
Months
Y1
1 260740
Children's Hospitals and Clinics of
Minnesota - Minneapolis
Yes 12
2 268128
University of Minnesota Masonic Children's
Hospital
Yes 0.1
Positions

ACGME Program Requirements for
Graduate Medical Education
in Pediatric Otolaryngology
ACGME-approved: June 10, 2012; effective: July 1, 2013
ACGME approved categorization: June 9, 2013; effective: July 1, 2014
ACGME approved focused revision: February 3, 2014; effective: July 1, 2014
Revised Common Program Requirements effective: July 1, 2015
Revised Common Program Requirements effective: July 1, 2016
Revised Common Program Requirements effective: July 1, 2017
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 1 of 27
ACGME Program Requirements for Graduate Medical Education
in Pediatric Otolaryngology
One-year Common Program Requirements are in BOLD
Where applicable, text in italics describes the underlying philosophy of the requirements in that
section. These philosophic statements are not program requirements and are therefore not
citable.
Introduction
Int.A. Residency and fellowship programs are essential dimensions of the
transformation of the medical student to the independent practitioner along
the continuum of medical education. They are physically, emotionally, and
intellectually demanding, and require longitudinally-concentrated effort on
the part of the resident or fellow.
The specialty education of physicians to practice independently is
experiential, and necessarily occurs within the context of the health care
delivery system. Developing the skills, knowledge, and attitudes leading to
proficiency in all the domains of clinical competency requires the resident
and fellow physician to assume personal responsibility for the care of
individual patients. For the resident and fellow, the essential learning
activity is interaction with patients under the guidance and supervision of
faculty members who give value, context, and meaning to those
interactions. As residents and fellows gain experience and demonstrate
growth in their ability to care for patients, they assume roles that permit
them to exercise those skills with greater independence. This concept--
graded and progressive responsibility--is one of the core tenets of
American graduate medical education. Supervision in the setting of
graduate medical education has the goals of assuring the provision of safe
and effective care to the individual patient; assuring each resident’s and
fellow’s development of the skills, knowledge, and attitudes required to
enter the unsupervised practice of medicine; and establishing a foundation
for continued professional growth.
Int.B. Pediatric otolaryngologists specialize in the medical and surgical management of
neonates, infants, children, and adolescents 18 years or younger, particularly
those with complex otolaryngologic problems and significant co-morbidities,
generally cared for in tertiary care pediatric institutions.
Int.C. The educational program in pediatric otolaryngology must be 12 months in
length.
(Core)
I. Institutions
I.A. Sponsoring Institution
One sponsoring institution must assume ultimate responsibility for the
program, as described in the Institutional Requirements, and this
responsibility extends to fellow assignments at all participating sites.
(Core)
*
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 2 of 27
The sponsoring institution and the program must ensure that the program
director has sufficient protected time and financial support for his or her
educational and administrative responsibilities to the program.
(Core)
I.A.1. The program must be based in a tertiary care pediatric institution where
the care of neonates and children can be readily coordinated with other
subspecialists.
(Core)
I.A.2. The sponsoring institution must also sponsor an Accreditation Council for
Graduate Medical Education (ACGME)-accredited otolaryngology
program.
(Core)
I.B. Participating Sites
I.B.1. There must be a program letter of agreement (PLA) between the
program and each participating site providing a required
assignment. The PLA must be renewed at least every five years.
(Core)
The PLA should:
I.B.1.a) identify the faculty who will assume both educational and
supervisory responsibilities for fellows;
(Detail)
I.B.1.b) specify their responsibilities for teaching, supervision, and
formal evaluation of fellows, as specified later in this
document;
(Detail)
I.B.1.c) specify the duration and content of the educational
experience; and,
(Detail)
I.B.1.d) state the policies and procedures that will govern fellow
education during the assignment.
(Detail)
I.B.2. The program director must submit any additions or deletions of
participating sites routinely providing an educational experience,
required for all fellows, of one month full time equivalent (FTE) or
more through the Accreditation Council for Graduate Medical
Education (ACGME) Accreditation Data System (ADS).
(Core)
II. Program Personnel and Resources
II.A. Program Director
II.A.1. There must be a single program director with authority and
accountability for the operation of the program. The sponsoring
institution’s GMEC must approve a change in program director.
(Core)
II.A.1.a) The program director must submit this change to the ACGME
via the ADS.
(Core)
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 3 of 27
II.A.2. Qualifications of the program director must include:
II.A.2.a) requisite specialty expertise and documented educational
and administrative experience acceptable to the Review
Committee;
(Core)
II.A.2.b) current certification in the subspecialty by the American
Board of Otolaryngology (ABOto), or subspecialty
qualifications that are acceptable to the Review Committee;
and,
(Core)
II.A.2.b).(1) The Review Committee only accepts ABOto certification in
otolaryngology.
(Core)
II.A.2.b).(2) The program director should have also completed a
pediatric otolaryngology fellowship.
(Core)
II.A.2.c) current medical licensure and appropriate medical staff
appointment.
(Core)
II.A.3. The program director must administer and maintain an educational
environment conducive to educating the fellows in each of the
ACGME competency areas.
(Core)
The program director must:
II.A.3.a) prepare and submit all information required and requested by
the ACGME;
(Core)
II.A.3.b) be familiar with and oversee compliance with ACGME and
Review Committee policies and procedures as outlined in the
ACGME Manual of Policies and Procedures;
(Detail)
II.A.3.c) obtain review and approval of the sponsoring institution’s
GMEC/DIO before submitting information or requests to the
ACGME, including:
(Core)
II.A.3.c).(1) all applications for ACGME accreditation of new
programs;
(Detail)
II.A.3.c).(2) changes in fellow complement;
(Detail)
II.A.3.c).(3) major changes in program structure or length of
training;
(Detail)
II.A.3.c).(4) progress reports requested by the Review Committee;
(Detail)
II.A.3.c).(5) requests for increases or any change to fellow duty
hours;
(Detail)
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 4 of 27
II.A.3.c).(6) voluntary withdrawals of ACGME-accredited
programs;
(Detail)
II.A.3.c).(7) requests for appeal of an adverse action; and,
(Detail)
II.A.3.c).(8) appeal presentations to a Board of Appeal or the
ACGME.
(Detail)
II.A.3.d) obtain DIO review and co-signature on all program
application forms, as well as any correspondence or
document submitted to the ACGME that addresses:
(Detail)
II.A.3.d).(1) program citations, and/or,
(Detail)
II.A.3.d).(2) request for changes in the program that would have
significant impact, including financial, on the program
or institution.
(Detail)
II.A.3.e) prepare and implement a supervision policy that specifies lines of
responsibility for fellows and faculty members, as well as for
residents and other learners.
(Core)
II.B. Faculty
II.B.1. There must be a sufficient number of faculty with documented
qualifications to instruct and supervise all fellows.
(Core)
II.B.2. The faculty must devote sufficient time to the educational program
to fulfill their supervisory and teaching responsibilities and
demonstrate a strong interest in the education of fellows.
(Core)
II.B.3. The physician faculty must have current certification in the
subspecialty by the American Board of Otolaryngology, or possess
qualifications judged acceptable to the Review Committee.
(Core)
II.B.3.a) The Review Committee only accepts ABOto certification in
otolaryngology.
(Core)
II.B.4. The physician faculty must possess current medical licensure and
appropriate medical staff appointment.
(Core)
II.B.5. The faculty must establish and maintain an environment of inquiry and
scholarship with an active research component.
(Core)
II.B.6. Scholarly activity of each core physician faculty member must include at
least one of the following
(Core)
II.B.6.a) funded research grants;
(Detail)
II.B.6.b) peer-reviewed publications; or,
(Detail)
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 5 of 27
II.B.6.c) presentations in regional or national conferences.
(Detail)
II.B.7. To enhance fellows’ educational experience, there must be participation
from appropriately-qualified faculty members from other related pediatric
disciplines, including:
(Core)
II.B.7.a) anesthesiology;
(Core)
II.B.7.b) audiology and speech pathology;
(Core)
II.B.7.c) child and adolescent psychiatry;
(Core)
II.B.7.d) gastroenterology;
(Core)
II.B.7.e) medical genetics;
(Core)
II.B.7.f) neonatology;
(Core)
II.B.7.g) neurology;
(Core)
II.B.7.h) pathology;
(Core)
II.B.7.i) plastic surgery;
(Core)
II.B.7.j) prenatal and fetal medicine;
(Core)
II.B.7.k) pulmonology;
(Core)
II.B.7.l) radiology; and,
(Core)
II.B.7.m) sleep medicine.
(Core)
II.C. Other Program Personnel
The institution and the program must jointly ensure the availability of all
necessary professional, technical, and clerical personnel for the effective
administration of the program.
(Core)
II.D. Resources
The institution and the program must jointly ensure the availability of
adequate resources for fellow education, as defined in the specialty
program requirements.
(Core)
II.D.1. Program resources must include:
II.D.1.a) inpatient and outpatient facilities.
(Core)
II.D.1.b) an emergency department;
(Core)
II.D.1.c) neonatal and pediatric intensive care units;
(Core)
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 6 of 27
II.D.1.d) facilities for the diagnostic assessment of infants and children with
otolaryngologic disorders, including audiologic, voice, speech,
language and developmental assessments; and,
(Core)
II.D.1.e) facilities to support clinical research.
(Core)
II.D.2. Fellows must be provided with prompt reliable systems for communication
and interaction with supervising physicians.
(Core)
II.E. Medical Information Access
Fellows must have ready access to specialty-specific and other appropriate
reference material in print or electronic format. Electronic medical literature
databases with search capabilities should be available.
(Detail)
III. Fellow Appointments
III.A. Eligibility Requirements – Fellowship Programs
All required clinical education for entry into ACGME-accredited fellowship
programs must be completed in an ACGME-accredited residency program,
or in an RCPSC-accredited or CFPC-accredited residency program located
in Canada.
(Core)
Prior to appointment in the program, fellows must have successfully completed
an otolaryngology residency accredited by the ACGME, or an otolaryngology
residency located in Canada and accredited by the RCPSC.
(Core)
III.A.1. Fellowship programs must receive verification of each entering
fellow’s level of competency in the required field using ACGME or
CanMEDS Milestones assessments from the core residency
program.
(Core)
III.A.2. Fellow Eligibility Exception
A Review Committee may grant the following exception to the
fellowship eligibility requirements:
An ACGME-accredited fellowship program may accept an
exceptionally qualified applicant**, who does not satisfy the
eligibility requirements listed in Sections III.A. and III.A.1., but who
does meet all of the following additional qualifications and
conditions:
(Core)
III.A.2.a) Assessment by the program director and fellowship selection
committee of the applicant’s suitability to enter the program,
based on prior training and review of the summative
evaluations of training in the core specialty; and
(Core)
III.A.2.b) Review and approval of the applicant’s exceptional
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 7 of 27
qualifications by the GMEC or a subcommittee of the GMEC;
and
(Core)
III.A.2.c) Satisfactory completion of the United States Medical
Licensing Examination (USMLE) Steps 1, 2, and, if the
applicant is eligible, 3, and;
(Core)
III.A.2.d) For an international graduate, verification of Educational
Commission for Foreign Medical Graduates (ECFMG)
certification; and,
(Core)
III.A.2.e) Applicants accepted by this exception must complete
fellowship Milestones evaluation (for the purposes of
establishment of baseline performance by the Clinical
Competency Committee), conducted by the receiving
fellowship program within six weeks of matriculation. This
evaluation may be waived for an applicant who has
completed an ACGME International-accredited residency
based on the applicant’s Milestones evaluation conducted at
the conclusion of the residency program.
(Core)
III.A.2.e).(1) If the trainee does not meet the expected level of
Milestones competency following entry into the
fellowship program, the trainee must undergo a period
of remediation, overseen by the Clinical Competency
Committee and monitored by the GMEC or a
subcommittee of the GMEC. This period of remediation
must not count toward time in fellowship training.
(Core)
** An exceptionally qualified applicant has (1) completed a non-
ACGME-accredited residency program in the core specialty, and (2)
demonstrated clinical excellence, in comparison to peers,
throughout training. Additional evidence of exceptional
qualifications is required, which may include one of the following:
(a) participation in additional clinical or research training in the
specialty or subspecialty; (b) demonstrated scholarship in the
specialty or subspecialty; (c) demonstrated leadership during or
after residency training; (d) completion of an ACGME-International-
accredited residency program.
III.A.3. The Review Committee for Otolaryngology does not allow exceptions
to the Eligibility Requirements for Fellowship Programs in Section
III.A.
(Core)
III.B. Number of Fellows
The program’s educational resources must be adequate to support the
number of fellows appointed to the program.
(Core)
III.B.1. The program director may not appoint more fellows than approved
by the Review Committee, unless otherwise stated in the specialty-
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 8 of 27
specific requirements.
(Core)
III.C. Other Learners
The presence of other learners, including otolaryngology residents, residents
from other specialties, unaccredited pediatric otolaryngology fellows, other
subspecialty fellows, PhD students, and nurse practitioners, must not interfere
with the appointed fellows’ education.
(Core)
IV. Educational Program
IV.A. The curriculum must contain the following educational components:
IV.A.1. Skills and competencies the fellow will be able to demonstrate at the
conclusion of the program. The program must distribute these skills
and competencies to fellows and faculty at least annually, in either
written or electronic form.
(Core)
IV.A.2. ACGME Competencies
The program must integrate the following ACGME competencies
into the curriculum:
(Core)
IV.A.2.a) Patient Care and Procedural Skills
IV.A.2.a).(1) Fellows must be able to provide patient care that is
compassionate, appropriate, and effective for the
treatment of health problems and the promotion of
health.
(Outcome)
IV.A.2.a).(2) Fellows must be able to competently perform all
medical, diagnostic, and surgical procedures
considered essential for the area of practice. Fellows:
(Outcome)
must demonstrate competence in:
IV.A.2.a).(2).(a) evaluating neonates, infants, children, and
adolescents 18 years and younger with congenital
abnormalities, infectious and inflammatory
disorders, and inherited and acquired conditions of
the head and neck, including hearing loss and other
communication impairments;
(Outcome)
IV.A.2.a).(2).(b) diagnosing and managing the medical and surgical
treatment of the aerodigestive tract, ear, nose,
sinus, throat, voice and speech, and head and neck
and disorders of neonates, infants, children, and
adolescents 18 years and younger; and,
(Outcome)
IV.A.2.a).(2).(c) performing procedures in the following domains
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 9 of 27
with an emphasis on neonates, infants, children
younger than three years of age, and children and
adolescents with significant co-morbidities as
defined by American Society of Anesthesiology
(ASA) status:
(Outcome)
IV.A.2.a).(2).(c).(i) closed and open airways;
(Outcome)
IV.A.2.a).(2).(c).(ii) congenital anomalies;
(Outcome)
IV.A.2.a).(2).(c).(iii) endoscopic airways;
(Outcome)
IV.A.2.a).(2).(c).(iv) facial plastics;
(Outcome)
IV.A.2.a).(2).(c).(v) facial trauma;
(Outcome)
IV.A.2.a).(2).(c).(vi) head and neck surgery;
(Outcome)
IV.A.2.a).(2).(c).(vii) otology;
(Outcome)
IV.A.2.a).(2).(c).(viii) rhinology; and,
(Outcome)
IV.A.2.a).(2).(c).(ix) complex and uncommon pediatric
procedures infrequently encountered in the
general practice of otolaryngology.
(Outcome)
IV.A.2.a).(3) Fellows must document surgical experience as assistant
surgeon, surgeon, and resident supervisor in the ACGME
Case Log System, recording patient age and ASA
classification for each documented case.
(Core)
IV.A.2.b) Medical Knowledge
Fellows must demonstrate knowledge of established and
evolving biomedical, clinical, epidemiological and social-
behavioral sciences, as well as the application of this
knowledge to patient care. Fellows:
(Outcome)
IV.A.2.b).(1) must demonstrate proficiency in their knowledge of
medical and surgical management of neonatal, infant,
childhood, and adolescent diseases of the head and neck
to a level appropriate for unsupervised practice as defined
by the didactic curriculum.
(Outcome)
IV.A.2.c) Practice-based Learning and Improvement
Fellows are expected to develop skills and habits to be able
to meet the following goals:
IV.A.2.c).(1) systematically analyze practice using quality
improvement methods, and implement changes with
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 10 of 27
the goal of practice improvement; and,
(Outcome)
IV.A.2.c).(2) locate, appraise, and assimilate evidence from
scientific studies related to their patients’ health
problems.
(Outcome)
IV.A.2.d) Interpersonal and Communication Skills
Fellows must demonstrate interpersonal and communication
skills that result in the effective exchange of information and
collaboration with patients, their families, and health
professionals.
(Outcome)
IV.A.2.e) Professionalism
Fellows must demonstrate a commitment to carrying out
professional responsibilities and an adherence to ethical
principles.
(Outcome)
IV.A.2.e).(1) Fellows must demonstrate competence in advocating for
quality patient care when facilitating patient management
in the home, school, or institutional setting.
(Outcome)
IV.A.2.f) Systems-based Practice
Fellows must demonstrate an awareness of and
responsiveness to the larger context and system of health
care, as well as the ability to call effectively on other
resources in the system to provide optimal health care.
(Outcome)
IV.A.3. Curriculum Organization and Fellow Experiences
IV.A.3.a) The didactic curriculum must include basic science, clinical, and
research conferences and seminars, as well as journal club
activities pertaining to pediatric otolaryngology.
(Core)
IV.A.3.a).(1) Didactic topics must include:
IV.A.3.a).(1).(a) developmental anatomy and physiology,
embryology, microbiology, oncology, and
psychology of the infant and child as related to the
head and neck;
(Detail)
IV.A.3.a).(1).(b) diagnosis and care of uncommon and complex
congenital and acquired conditions involving the
aerodigestive tract, nose and paranasal sinuses,
and ear, as well as diseases and disorders of the
laryngotracheal complex and the head and neck;
(Detail)
IV.A.3.a).(1).(c) diagnosis, treatment, and management of
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 11 of 27
childhood disorders of hearing, language, speech,
and voice; and,
(Detail)
IV.A.3.a).(1).(d) genetics.
(Detail)
IV.A.3.a).(2) Quality improvement conferences must take place at least
quarterly.
(Detail)
IV.A.3.a).(3) Fellows must participate in planning and conducting
conferences.
(Detail)
IV.A.3.a).(4) Both faculty members and fellows must attend and
participate in multidisciplinary conferences.
(Detail)
IV.A.3.a).(5) Faculty and fellow attendance at conferences must be
documented.
(Detail)
IV.A.3.b) Fellows’ clinical experiences must include:
IV.A.3.b).(1) participation in a multispecialty, interdisciplinary team to
manage and treat conditions for at least three of the
following: cochlear implant, craniofacial disorders, tumors,
or vascular anomalies; and,
(Core)
IV.A.3.b).(2) attendance at a minimum of four clinic sessions per month.
(Detail)
IV.B. Fellows’ Scholarly Activities
IV.B.1. Fellows’ scholarly activity initiated or completed during the program,
including scientific study, production of review articles or chapters, or
creation of online educational activities, must be documented.
(Outcome)
V. Evaluation
V.A. Fellow Evaluation
V.A.1. The program director must appoint the Clinical Competency
Committee.
(Core)
V.A.1.a) At a minimum the Clinical Competency Committee must be
composed of three members of the program faculty.
(Core)
V.A.1.a).(1) The program director may appoint additional members
of the Clinical Competency Committee.
V.A.1.a).(1).(a) These additional members must be physician
faculty members from the same program or
other programs, or other health professionals
who have extensive contact and experience
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 12 of 27
with the program’s fellows in patient care and
other health care settings.
(Core)
V.A.1.a).(1).(b) Chief residents who have completed core
residency programs in their specialty and are
eligible for specialty board certification may be
members of the Clinical Competency
Committee.
(Core)
V.A.1.b) There must be a written description of the responsibilities of
the Clinical Competency Committee.
(Core)
V.A.1.b).(1) The Clinical Competency Committee should:
V.A.1.b).(1).(a) review all fellow evaluations semi-annually;
(Core)
V.A.1.b).(1).(b) prepare and ensure the reporting of Milestones
evaluations of each fellow semi-annually to
ACGME; and,
(Core)
V.A.1.b).(1).(c) advise the program director regarding fellow
progress, including promotion, remediation,
and dismissal.
(Detail)
V.A.2. Formative Evaluation
V.A.2.a) The faculty must evaluate fellow performance in a timely
manner.
(Core)
V.A.2.b) The program must:
V.A.2.b).(1) provide objective assessments of competence in
patient care and procedural skills, medical knowledge,
practice-based learning and improvement,
interpersonal and communication skills,
professionalism, and systems-based practice based
on the specialty-specific Milestones;
(Core)
V.A.2.b).(2) use multiple evaluators (e.g., faculty, peers, patients,
self, and other professional staff); and,
(Detail)
V.A.2.b).(3) provide each fellow with documented semiannual
evaluation of performance with feedback.
(Core)
V.A.2.c) The evaluations of fellow performance must be accessible for
review by the fellow, in accordance with institutional policy.
(Detail)
V.A.2.d) The program director must meet with each fellow in person to
review his or her cumulative operative experience and Case Log
data at least semiannually to ensure balanced progress towards
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 13 of 27
achieving experience with a variety and complexity of surgical
procedures.
(Core)
V.A.3. Summative Evaluation
V.A.3.a) The specialty-specific Milestones must be used as one of the
tools to ensure fellows are able to practice core professional
activities without supervision upon completion of the
program.
(Core)
V.A.3.b) The program director must provide a summative evaluation
for each fellow upon completion of the program.
(Core)
This evaluation must:
V.A.3.b).(1) become part of the fellow’s permanent record
maintained by the institution, and must be accessible
for review by the fellow in accordance with
institutional policy;
(Detail)
V.A.3.b).(2) document the fellow’s performance during their
education; and,
(Detail)
V.A.3.b).(3) verify that the fellow has demonstrated sufficient
competence to enter practice without direct
supervision.
(Detail)
V.B. Faculty Evaluation
V.B.1. At least annually, the program must evaluate faculty performance as
it relates to the educational program.
(Core)
V.B.2. These evaluations should include a review of the faculty’s clinical
teaching abilities, commitment to the educational program, clinical
knowledge, professionalism, and scholarly activities.
(Detail)
V.C. Program Evaluation and Improvement
V.C.1. The program director must appoint the Program Evaluation
Committee (PEC).
(Core)
V.C.1.a) The Program Evaluation Committee:
V.C.1.a).(1) must be composed of at least two program faculty
members and should include at least one fellow;
(Core)
V.C.1.a).(2) must have a written description of its responsibilities;
and,
(Core)
V.C.1.a).(3) should participate actively in:
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 14 of 27
V.C.1.a).(3).(a) planning, developing, implementing, and
evaluating educational activities of the
program;
(Detail)
V.C.1.a).(3).(b) reviewing and making recommendations for
revision of competency-based curriculum goals
and objectives;
(Detail)
V.C.1.a).(3).(c) addressing areas of non-compliance with
ACGME standards; and,
(Detail)
V.C.1.a).(3).(d) reviewing the program annually using
evaluations of faculty, fellows, and others, as
specified below.
(Detail)
V.C.2. The program, through the PEC, must document formal, systematic
evaluation of the curriculum at least annually, and is responsible for
rendering a written, annual program evaluation.
(Core)
The program must monitor and track each of the following areas:
V.C.2.a) fellow performance;
(Core)
V.C.2.b) faculty development; and,
(Core)
V.C.2.c) progress on the previous year’s action plan(s).
(Core)
V.C.3. The PEC must prepare a written plan of action to document
initiatives to improve performance in one or more of the areas listed
in section V.C.2., as well as delineate how they will be measured and
monitored.
(Core)
V.C.3.a) The action plan should be reviewed and approved by the
teaching faculty and documented in meeting minutes.
(Detail)
V.C.4. The faculty must meet at least annually to review program goals and
objectives and program effectiveness in achieving them. At least one
fellow should participate in these reviews.
(Detail)
VI. The Learning and Working Environment
Fellowship education must occur in the context of a learning and working
environment that emphasizes the following principles:
Excellence in the safety and quality of care rendered to patients by fellows
today
Excellence in the safety and quality of care rendered to patients by today’s
fellows in their future practice
Excellence in professionalism through faculty modeling of:
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 15 of 27
o the effacement of self-interest in a humanistic environment that supports
the professional development of physicians
o the joy of curiosity, problem-solving, intellectual rigor, and discovery
Commitment to the well-being of the students, residents/fellows, faculty
members, and all members of the health care team
VI.A. Patient Safety, Quality Improvement, Supervision, and Accountability
VI.A.1. Patient Safety and Quality Improvement
All physicians share responsibility for promoting patient safety and
enhancing quality of patient care. Graduate medical education must
prepare fellows to provide the highest level of clinical care with
continuous focus on the safety, individual needs, and humanity of
their patients. It is the right of each patient to be cared for by fellows
who are appropriately supervised; possess the requisite knowledge,
skills, and abilities; understand the limits of their knowledge and
experience; and seek assistance as required to provide optimal
patient care.
Fellows must demonstrate the ability to analyze the care they
provide, understand their roles within health care teams, and play an
active role in system improvement processes. Graduating fellows
will apply these skills to critique their future unsupervised practice
and effect quality improvement measures.
It is necessary for fellows and faculty members to consistently work
in a well-coordinated manner with other health care professionals to
achieve organizational patient safety goals.
VI.A.1.a) Patient Safety
VI.A.1.a).(1) Culture of Safety
A culture of safety requires continuous identification
of vulnerabilities and a willingness to transparently
deal with them. An effective organization has formal
mechanisms to assess the knowledge, skills, and
attitudes of its personnel toward safety in order to
identify areas for improvement.
VI.A.1.a).(1).(a) The program, its faculty, residents, and fellows
must actively participate in patient safety
systems and contribute to a culture of safety.
(Core)
VI.A.1.a).(1).(b) The program must have a structure that
promotes safe, interprofessional, team-based
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 16 of 27
care.
(Core)
VI.A.1.a).(2) Education on Patient Safety
Programs must provide formal educational activities
that promote patient safety-related goals, tools, and
techniques.
(Core)
VI.A.1.a).(3) Patient Safety Events
Reporting, investigation, and follow-up of adverse
events, near misses, and unsafe conditions are pivotal
mechanisms for improving patient safety, and are
essential for the success of any patient safety
program. Feedback and experiential learning are
essential to developing true competence in the ability
to identify causes and institute sustainable systems-
based changes to ameliorate patient safety
vulnerabilities.
VI.A.1.a).(3).(a) Residents, fellows, faculty members, and other
clinical staff members must:
VI.A.1.a).(3).(a).(i) know their responsibilities in reporting
patient safety events at the clinical site;
(Core)
VI.A.1.a).(3).(a).(ii) know how to report patient safety
events, including near misses, at the
clinical site; and,
(Core)
VI.A.1.a).(3).(a).(iii) be provided with summary information
of their institution’s patient safety
reports.
(Core)
VI.A.1.a).(3).(b) Fellows must participate as team members in
real and/or simulated interprofessional clinical
patient safety activities, such as root cause
analyses or other activities that include
analysis, as well as formulation and
implementation of actions.
(Core)
VI.A.1.a).(4) Fellow Education and Experience in Disclosure of
Adverse Events
Patient-centered care requires patients, and when
appropriate families, to be apprised of clinical
situations that affect them, including adverse events.
This is an important skill for faculty physicians to
model, and for fellows to develop and apply.
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 17 of 27
VI.A.1.a).(4).(a) All fellows must receive training in how to
disclose adverse events to patients and
families.
(Core)
VI.A.1.a).(4).(b) Fellows should have the opportunity to
participate in the disclosure of patient safety
events, real or simulated.
(Detail)
VI.A.1.b) Quality Improvement
VI.A.1.b).(1) Education in Quality Improvement
A cohesive model of health care includes quality-
related goals, tools, and techniques that are necessary
in order for health care professionals to achieve
quality improvement goals.
VI.A.1.b).(1).(a) Fellows must receive training and experience in
quality improvement processes, including an
understanding of health care disparities.
(Core)
VI.A.1.b).(2) Quality Metrics
Access to data is essential to prioritizing activities for
care improvement and evaluating success of
improvement efforts.
VI.A.1.b).(2).(a) Fellows and faculty members must receive data
on quality metrics and benchmarks related to
their patient populations.
(Core)
VI.A.1.b).(3) Engagement in Quality Improvement Activities
Experiential learning is essential to developing the
ability to identify and institute sustainable systems-
based changes to improve patient care.
VI.A.1.b).(3).(a) Fellows must have the opportunity to
participate in interprofessional quality
improvement activities.
(Core)
VI.A.1.b).(3).(a).(i) This should include activities aimed at
reducing health care disparities.
(Detail)
VI.A.2. Supervision and Accountability
VI.A.2.a) Although the attending physician is ultimately responsible for
the care of the patient, every physician shares in the
responsibility and accountability for their efforts in the
provision of care. Effective programs, in partnership with
their Sponsoring Institutions, define, widely communicate,
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 18 of 27
and monitor a structured chain of responsibility and
accountability as it relates to the supervision of all patient
care.
Supervision in the setting of graduate medical education
provides safe and effective care to patients; ensures each
fellow’s development of the skills, knowledge, and attitudes
required to enter the unsupervised practice of medicine; and
establishes a foundation for continued professional growth.
VI.A.2.a).(1) Each patient must have an identifiable and
appropriately-credentialed and privileged attending
physician (or licensed independent practitioner as
specified by the applicable Review Committee) who is
responsible and accountable for the patient’s care.
(Core)
VI.A.2.a).(1).(a) This information must be available to fellows,
faculty members, other members of the health
care team, and patients.
(Core)
VI.A.2.a).(1).(b) Fellows and faculty members must inform each
patient of their respective roles in that patient’s
care when providing direct patient care.
(Core)
VI.A.2.b) Supervision may be exercised through a variety of methods.
For many aspects of patient care, the supervising physician
may be a more advanced fellow. Other portions of care
provided by the fellow can be adequately supervised by the
immediate availability of the supervising faculty member or
fellow physician, either on site or by means of telephonic
and/or electronic modalities. Some activities require the
physical presence of the supervising faculty member. In
some circumstances, supervision may include post-hoc
review of fellow-delivered care with feedback.
VI.A.2.b).(1) The program must demonstrate that the appropriate
level of supervision in place for all fellows is based on
each fellow’s level of training and ability, as well as
patient complexity and acuity. Supervision may be
exercised through a variety of methods, as appropriate
to the situation.
(Core)
VI.A.2.c) Levels of Supervision
To promote oversight of fellow supervision while providing
for graded authority and responsibility, the program must use
the following classification of supervision:
(Core)
VI.A.2.c).(1) Direct Supervision – the supervising physician is
physically present with the fellow and patient.
(Core)
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 19 of 27
VI.A.2.c).(2) Indirect Supervision:
VI.A.2.c).(2).(a) with Direct Supervision immediately available –
the supervising physician is physically within
the hospital or other site of patient care, and is
immediately available to provide Direct
Supervision.
(Core)
VI.A.2.c).(2).(b) with Direct Supervision available – the
supervising physician is not physically present
within the hospital or other site of patient care,
but is immediately available by means of
telephonic and/or electronic modalities, and is
available to provide Direct Supervision.
(Core)
VI.A.2.c).(3) Oversight – the supervising physician is available to
provide review of procedures/encounters with
feedback provided after care is delivered.
(Core)
VI.A.2.d) The privilege of progressive authority and responsibility,
conditional independence, and a supervisory role in patient
care delegated to each fellow must be assigned by the
program director and faculty members.
(Core)
VI.A.2.d).(1) The program director must evaluate each fellow’s
abilities based on specific criteria, guided by the
Milestones.
(Core)
VI.A.2.d).(2) Faculty members functioning as supervising
physicians must delegate portions of care to fellows
based on the needs of the patient and the skills of
each fellow.
(Core)
VI.A.2.d).(3) Fellows should serve in a supervisory role to residents
or junior fellows in recognition of their progress
toward independence, based on the needs of each
patient and the skills of the individual resident or
fellow.
(Detail)
VI.A.2.e) Programs must set guidelines for circumstances and events
in which fellows must communicate with the supervising
faculty member(s).
(Core)
VI.A.2.e).(1) Each fellow must know the limits of their scope of
authority, and the circumstances under which the
fellow is permitted to act with conditional
independence.
(Outcome)
VI.A.2.f) Faculty supervision assignments must be of sufficient
duration to assess the knowledge and skills of each fellow
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 20 of 27
and to delegate to the fellow the appropriate level of patient
care authority and responsibility.
(Core)
VI.B. Professionalism
VI.B.1. Programs, in partnership with their Sponsoring Institutions, must
educate fellows and faculty members concerning the professional
responsibilities of physicians, including their obligation to be
appropriately rested and fit to provide the care required by their
patients.
(Core)
VI.B.2. The learning objectives of the program must:
VI.B.2.a) be accomplished through an appropriate blend of supervised
patient care responsibilities, clinical teaching, and didactic
educational events;
(Core)
VI.B.2.b) be accomplished without excessive reliance on fellows to
fulfill non-physician obligations; and,
(Core)
VI.B.2.c) ensure manageable patient care responsibilities.
(Core)
VI.B.3. The program director, in partnership with the Sponsoring Institution,
must provide a culture of professionalism that supports patient
safety and personal responsibility.
(Core)
VI.B.4. Fellows and faculty members must demonstrate an understanding
of their personal role in the:
VI.B.4.a) provision of patient- and family-centered care;
(Outcome)
VI.B.4.b) safety and welfare of patients entrusted to their care,
including the ability to report unsafe conditions and adverse
events;
(Outcome)
VI.B.4.c) assurance of their fitness for work, including:
(Outcome)
VI.B.4.c).(1) management of their time before, during, and after
clinical assignments; and,
(Outcome)
VI.B.4.c).(2) recognition of impairment, including from illness,
fatigue, and substance use, in themselves, their peers,
and other members of the health care team.
(Outcome)
VI.B.4.d) commitment to lifelong learning;
(Outcome)
VI.B.4.e) monitoring of their patient care performance improvement
indicators; and,
(Outcome)
VI.B.4.f) accurate reporting of clinical and educational work hours,
patient outcomes, and clinical experience data.
(Outcome)
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 21 of 27
VI.B.5. All fellows and faculty members must demonstrate responsiveness
to patient needs that supersedes self-interest. This includes the
recognition that under certain circumstances, the best interests of
the patient may be served by transitioning that patient’s care to
another qualified and rested provider.
(Outcome)
VI.B.6. Programs must provide a professional, respectful, and civil
environment that is free from mistreatment, abuse, or coercion of
students, residents/fellows, faculty, and staff. Programs, in
partnership with their Sponsoring Institutions, should have a
process for education of fellows and faculty regarding
unprofessional behavior and a confidential process for reporting,
investigating, and addressing such concerns.
(Core)
VI.C. Well-Being
In the current health care environment, fellows and faculty members are at
increased risk for burnout and depression. Psychological, emotional, and
physical well-being are critical in the development of the competent,
caring, and resilient physician. Self-care is an important component of
professionalism; it is also a skill that must be learned and nurtured in the
context of other aspects of fellowship training. Programs, in partnership
with their Sponsoring Institutions, have the same responsibility to address
well-being as they do to evaluate other aspects of fellow competence.
VI.C.1. This responsibility must include:
VI.C.1.a) efforts to enhance the meaning that each fellow finds in the
experience of being a physician, including protecting time
with patients, minimizing non-physician obligations,
providing administrative support, promoting progressive
autonomy and flexibility, and enhancing professional
relationships;
(Core)
VI.C.1.b) attention to scheduling, work intensity, and work
compression that impacts fellow well-being;
(Core)
VI.C.1.c) evaluating workplace safety data and addressing the safety of
fellows and faculty members;
(Core)
VI.C.1.d) policies and programs that encourage optimal fellow and
faculty member well-being; and,
(Core)
VI.C.1.d).(1) Fellows must be given the opportunity to attend
medical, mental health, and dental care appointments,
including those scheduled during their working hours.
(Core)
VI.C.1.e) attention to fellow and faculty member burnout, depression,
and substance abuse. The program, in partnership with its
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 22 of 27
Sponsoring Institution, must educate faculty members and
fellows in identification of the symptoms of burnout,
depression, and substance abuse, including means to assist
those who experience these conditions. Fellows and faculty
members must also be educated to recognize those
symptoms in themselves and how to seek appropriate care.
The program, in partnership with its Sponsoring Institution,
must:
(Core)
VI.C.1.e).(1) encourage fellows and faculty members to alert the
program director or other designated personnel or
programs when they are concerned that another
resident, fellow, or faculty member may be displaying
signs of burnout, depression, substance abuse,
suicidal ideation, or potential for violence;
(Core)
VI.C.1.e).(2) provide access to appropriate tools for self-screening;
and,
(Core)
VI.C.1.e).(3) provide access to confidential, affordable mental
health assessment, counseling, and treatment,
including access to urgent and emergent care 24
hours a day, seven days a week.
(Core)
VI.C.2. There are circumstances in which fellows may be unable to attend
work, including but not limited to fatigue, illness, and family
emergencies. Each program must have policies and procedures in
place that ensure coverage of patient care in the event that a fellow
may be unable to perform their patient care responsibilities. These
policies must be implemented without fear of negative
consequences for the fellow who is unable to provide the clinical
work.
(Core)
VI.D. Fatigue Mitigation
VI.D.1. Programs must:
VI.D.1.a) educate all faculty members and fellows to recognize the
signs of fatigue and sleep deprivation;
(Core)
VI.D.1.b) educate all faculty members and fellows in alertness
management and fatigue mitigation processes; and,
(Core)
VI.D.1.c) encourage fellows to use fatigue mitigation processes to
manage the potential negative effects of fatigue on patient
care and learning.
(Detail)
VI.D.2. Each program must ensure continuity of patient care, consistent
with the program’s policies and procedures referenced in VI.C.2, in
the event that a fellow may be unable to perform their patient care
responsibilities due to excessive fatigue.
(Core)
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 23 of 27
VI.D.3. The program, in partnership with its Sponsoring Institution, must
ensure adequate sleep facilities and safe transportation options for
fellows who may be too fatigued to safely return home.
(Core)
VI.E. Clinical Responsibilities, Teamwork, and Transitions of Care
VI.E.1. Clinical Responsibilities
The clinical responsibilities for each fellow must be based on PGY
level, patient safety, fellow ability, severity and complexity of patient
illness/condition, and available support services.
(Core)
VI.E.1.a) The workload associated with optimal clinical care of surgical
patients is a continuum from the moment of admission to the point
of discharge.
(Detail)
VI.E.1.b) During the fellowship education process, surgical teams should be
made up of attending surgeons, fellows, residents at various PGY
levels, medical students (when appropriate), and other health care
providers.
(Detail)
VI.E.1.c) The work of the caregiver team should be assigned to team
members based on each individual’s level of education,
experience, and competence.
(Detail)
VI.E.2. Teamwork
Fellows must care for patients in an environment that maximizes
communication. This must include the opportunity to work as a
member of effective interprofessional teams that are appropriate to
the delivery of care in the specialty and larger health system.
(Core)
VI.E.2.a) Effective surgical practices entail the involvement of members with
a mix of complementary skills and attributes (physicians, nurses,
and other staff). Success requires both an unwavering mutual
respect for those skills and contributions, and a shared
commitment to the process of patient care.
(Detail)
VI.E.2.b) Fellows must collaborate with fellow surgical residents, and with
especially faculty, other physicians outside of their specialty, and
non-traditional health care providers to best formulate treatment
plans for an increasingly diverse patient population.
(Detail)
VI.E.2.c) Fellows must assume personal responsibility to complete all tasks
to which they are assigned (or which they voluntarily assume) in a
timely fashion. These tasks must be completed within the hours
assigned, or, if that is not possible, fellows must learn and utilize
the established methods for handing off remaining tasks to
another member of the fellow team so that patient care is not
compromised.
(Detail)
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 24 of 27
VI.E.2.d) Lines of authority should be defined by programs, and all fellows
must have a working knowledge of expected reporting
relationships to maximize quality care and patient safety.
(Detail)
VI.E.3. Transitions of Care
VI.E.3.a) Programs must design clinical assignments to optimize
transitions in patient care, including their safety, frequency,
and structure.
(Core)
VI.E.3.b) Programs, in partnership with their Sponsoring Institutions,
must ensure and monitor effective, structured hand-over
processes to facilitate both continuity of care and patient
safety.
(Core)
VI.E.3.c) Programs must ensure that fellows are competent in
communicating with team members in the hand-over process.
(Outcome)
VI.E.3.d) Programs and clinical sites must maintain and communicate
schedules of attending physicians and fellows currently
responsible for care.
(Core)
VI.E.3.e) Each program must ensure continuity of patient care,
consistent with the program’s policies and procedures
referenced in VI.C.2, in the event that a fellow may be unable
to perform their patient care responsibilities due to excessive
fatigue or illness, or family emergency.
(Core)
VI.F. Clinical Experience and Education
Programs, in partnership with their Sponsoring Institutions, must design
an effective program structure that is configured to provide fellows with
educational and clinical experience opportunities, as well as reasonable
opportunities for rest and personal activities.
VI.F.1. Maximum Hours of Clinical and Educational Work per Week
Clinical and educational work hours must be limited to no more than
80 hours per week, averaged over a four-week period, inclusive of all
in-house clinical and educational activities, clinical work done from
home, and all moonlighting.
(Core)
VI.F.2. Mandatory Time Free of Clinical Work and Education
VI.F.2.a) The program must design an effective program structure that
is configured to provide fellows with educational
opportunities, as well as reasonable opportunities for rest
and personal well-being.
(Core)
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 25 of 27
VI.F.2.b) Fellows should have eight hours off between scheduled
clinical work and education periods.
(Detail)
VI.F.2.b).(1) There may be circumstances when fellows choose to
stay to care for their patients or return to the hospital
with fewer than eight hours free of clinical experience
and education. This must occur within the context of
the 80-hour and the one-day-off-in-seven
requirements.
(Detail)
VI.F.2.c) Fellows must have at least 14 hours free of clinical work and
education after 24 hours of in-house call.
(Core)
VI.F.2.d) Fellows must be scheduled for a minimum of one day in
seven free of clinical work and required education (when
averaged over four weeks). At-home call cannot be assigned
on these free days.
(Core)
VI.F.3. Maximum Clinical Work and Education Period Length
VI.F.3.a) Clinical and educational work periods for fellows must not
exceed 24 hours of continuous scheduled clinical
assignments.
(Core)
VI.F.3.a).(1) Up to four hours of additional time may be used for
activities related to patient safety, such as providing
effective transitions of care, and/or fellow education.
(Core)
VI.F.3.a).(1).(a) Additional patient care responsibilities must not
be assigned to a fellow during this time.
(Core)
VI.F.4. Clinical and Educational Work Hour Exceptions
VI.F.4.a) In rare circumstances, after handing off all other
responsibilities, a fellow, on their own initiative, may elect to
remain or return to the clinical site in the following
circumstances:
VI.F.4.a).(1) to continue to provide care to a single severely ill or
unstable patient;
(Detail)
VI.F.4.a).(2) humanistic attention to the needs of a patient or
family; or,
(Detail)
VI.F.4.a).(3) to attend unique educational events.
(Detail)
VI.F.4.b) These additional hours of care or education will be counted
toward the 80-hour weekly limit.
(Detail)
VI.F.4.c) A Review Committee may grant rotation-specific exceptions
Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 26 of 27
for up to 10 percent or a maximum of 88 clinical and
educational work hours to individual programs based on a
sound educational rationale.
The Review Committee for Otolaryngology will not consider
requests for exceptions to the 80-hour limit to the fellows’ work
week.
VI.F.4.c).(1) In preparing a request for an exception, the program
director must follow the clinical and educational work
hour exception policy from the ACGME Manual of
Policies and Procedures.
(Core)
VI.F.4.c).(2) Prior to submitting the request to the Review
Committee, the program director must obtain approval
from the Sponsoring Institution’s GMEC and DIO.
(Core)
VI.F.5. Moonlighting
VI.F.5.a) Moonlighting must not interfere with the ability of the fellow
to achieve the goals and objectives of the educational
program, and must not interfere with the fellow’s fitness for
work nor compromise patient safety.
(Core)
VI.F.5.b) Time spent by fellows in internal and external moonlighting
(as defined in the ACGME Glossary of Terms) must be
counted toward the 80-hour maximum weekly limit.
(Core)
VI.F.6. In-House Night Float
Night float must occur within the context of the 80-hour and one-
day-off-in-seven requirements.
(Core)
VI.F.6.a) The Review Committee for Otolaryngology will not permit night
float.
VI.F.7. Maximum In-House On-Call Frequency
Fellows must be scheduled for in-house call no more frequently than
every third night (when averaged over a four-week period).
(Core)
VI.F.8. At-Home Call
VI.F.8.a) Time spent on patient care activities by fellows on at-home
call must count toward the 80-hour maximum weekly limit.
The frequency of at-home call is not subject to the every-
third-night limitation, but must satisfy the requirement for one
day in seven free of clinical work and education, when
averaged over four weeks.
(Core)
VI.F.8.a).(1) At-home call must not be so frequent or taxing as to

Pediatric Otolaryngology
©2017 Accreditation Council for Graduate Medical Education (ACGME) Page 27 of 27
preclude rest or reasonable personal time for each
fellow.
(Core)
VI.F.8.b) Fellows are permitted to return to the hospital while on at-
home call to provide direct care for new or established
patients. These hours of inpatient patient care must be
included in the 80-hour maximum weekly limit.
(Detail)
***
*Core Requirements: Statements that define structure, resource, or process elements essential to every
graduate medical educational program.
Detail Requirements: Statements that describe a specific structure, resource, or process, for achieving
compliance with a Core Requirement. Programs and sponsoring institutions in substantial compliance
with the Outcome Requirements may utilize alternative or innovative approaches to meet Core
Requirements.
Outcome Requirements: Statements that specify expected measurable or observable attributes
(knowledge, abilities, skills, or attitudes) of residents or fellows at key stages of their graduate medical
education.
Osteopathic Recognition
For programs seeking Osteopathic Recognition for the entire program, or for a track within the
program, the Osteopathic Recognition Requirements are also applicable.
(http://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/Osteopathic_Recogniton_Requirements.pdf)
