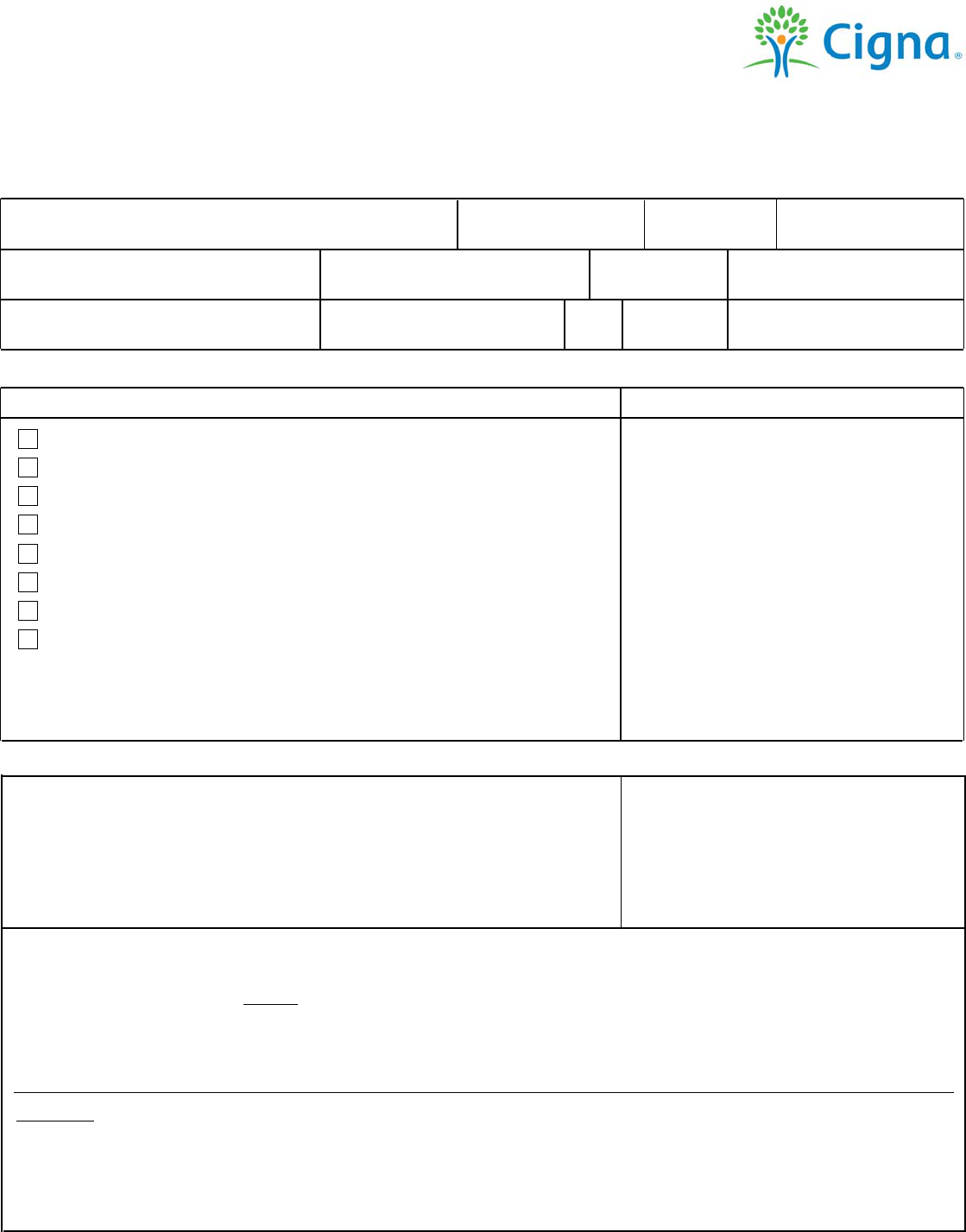
Cigna Medicare Advantage Non Contracted
Provider Appeals and Disputes Form
Complete the top section of this form completely and legibly. Check the box that most closely describes your
appeal reason. Be sure to include any supporting documentation, as indicated below. Requests received without
required information cannot be processed.
Request for appeal or dispute
Customer First Name: MI: Customer Last Name:
Customer's ID Number:
Date of Birth:
Claim Number:
Date(s) of Service:
Provider Name / Contact Name:
Provider NPI:
Provider Telephone Number:
Address: City:
State: Zip Code:
Provider's Contact Email:
Non Contracted Provider Appeals:
Reason for appeal:
Submit appeals to:
Medical Necessity and/or Level of Care Denial
Denied for no authorization (including OON denials)
Denied for no referral
DRG Payment Discrepancy
Downcoding Discrepancy
Overpayment Recovery Issue
Claim Bundling Discrepancy
Lack of Medical Records Denial
For payment issues related to Medicare allowable rates - see below.
Cigna Medicare Advantage Appeals
PO Box 188081
Chattanooga, TN 37422
Fax #: 855-350-8671
For all Non Contracted Provider
Appeals a completed Waiver of Liability
is required in order to process your
appeal. The Waiver of Liability
Statement must be signed. Your appeal
request will not be considered without
receipt of a signed Waiver of Liability
Statement. You can either mail or fax
your completed request, including the
attached Waiver of Liability.
Non Contracted Provider Payment Disputes:
A non-contracted provider is also permitted to request an independent
review if the amount paid for a covered service is less than the amount
that would have been paid under original Medicare.
For all other reasons, refer to the Appeal Request Reasons and address/fax
above.
Submit disputes to:
Cigna Medicare Services
Attn: Medicare Claims Department
Non Contracted Provider
Payment Disputes
PO Box 20002
Nashville, TN 37202
Note: If you have multiple appeal requests for the same health care professional and payment issue, please indicate this in
the notes below and include a list of the following: Customer ID #, Claim #, and date of service. If the issue requires
supporting documentation as noted above, it must be included for each individual appeal. You may use the space
starting on the next page to briefly describe your reason for appeal.
Definitions
Non Contracted Provider Appeal: A disagreement when the Plan is denying or recouping part or all of a payment for which the non-contracted
provider asked, such as for DRG coding, medical necessity, inpatient level of care determination, bundling rules, or emergency facility charges.
Appeals (reconsiderations) from a non-contracted provider must follow the regulations outlined at 42 CFR §422 Subpart M.
Non Contracted Provider Dispute: A disagreement about the amount that a non-contracted provider could have collected if the beneficiary
were in original Medicare.
All Cigna products and services are provided exclusively by or through operating subsidiaries of Cigna Corporation. The Cigna name, logos, and
other Cigna marks are owned by Cigna Intellectual Property, Inc © 2021
PCOMM-2021-1537
924661 11/2021
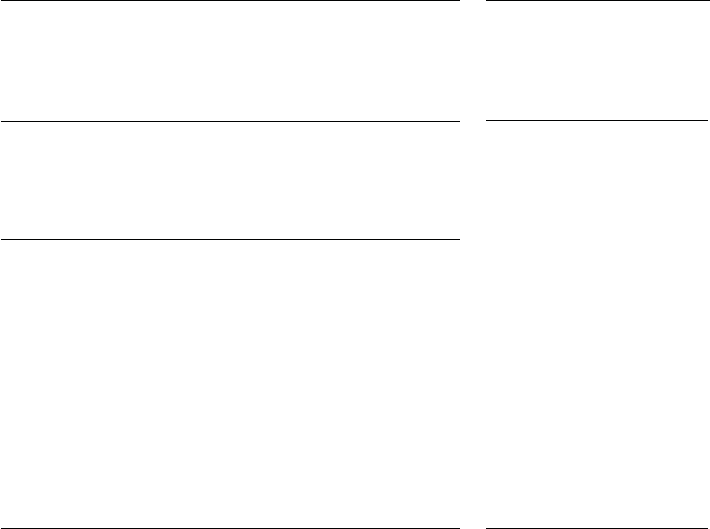
Waiver of Liability Statement
Enrollee's Name Enrollee ID Number
Provider
Date of Service
Health Plan
I hereby waive any right to collect payment from the above-mentioned enrollee for the
aforementioned services for which payment has been denied by the above-referenced health plan.
I understand that the signing of this waiver does not negate my right to request further appeal
under 42 CFR §422.600.
Signature Date
